India's Nutrition
India's Nutrition Context
India continues to face a double burden of malnutrition (DBM) as shown by the Comprehensive National Nutrition Survey 2016-2018 (CNNS) published by the Indian Ministry of Health and Family Welfare, with UNICEF and the Population Council, as well as by the 2019 Lancet series on the DBM. In the Lancet series DBM is defined as the simultaneous manifestation of both undernutrition and overweight and obesity.
Malnutrition not only directly affects people’s physical growth and health as well as their cognitive development and abilities, it has also been identified as one of the principal limitations of India’s global economic potential (Copenhagen consensus, 2012). The costs of malnutrition are enormous;
- Adults who were undernourished as children earn at least 20% less than those who were not;
- Undernutrition and micro-nutrient deficiencies cost societies up to $2.1 trillion per year;
- The cost of treating overweight or obesity is equal to 4-9% of a country’s Gross Domestic Product (GDP);
- Asia and Africa lose 11% of Gross National Product (GNP) every year owing to poor nutrition.
The opportunities are equally enormous; cost-benefit ratio analyses of nutrition interventions to reduce stunting in the first year of life report a monetary return (higher wages) later in life of 18:1 per child, and similar analyses found that a 1 cm increase in adult height due to nutrition interventions was associated with a 4% increase in wages for men, and 6% for women.
In recognition of the remaining challenges in nutrition, in early 2018, the Government of India launched the National Nutrition Mission (NNM), also known as POSHAN Abhiyaan, with ambitious reduction targets. But while it is encouraging that India has set NNM targets to reduce malnutrition, the trends up to 2017 indicate that substantially higher rates of annual improvement will be needed for all malnutrition indicators in most states in order to achieve the Indian 2022 targets, as well as the global 2030 goals set by WHO and UNICEF.
Targets set by the National Nutrition Mission for 2022 and WHO and UNICEF for 2030
National Nutrition Mission 2022 targets
- Low birthweight: 2 percentage point reduction in prevalence annually from 2017 to 2022
- Child stunting*: prevalence of 25% in 2022
- Child underweight*: 2 percentage point reduction in prevalence annually from 2017 to 2022
- Anaemia†: 3 percentage point reduction in prevalence annually in children younger than 5 years and in women 15–49 years of age from 2017 to 2022
WHO and UNICEF 2030 targets
- Low birthweight: 30% reduction in prevalence from 2012 to 2030
- Child stunting‡: 50% reduction in number of children younger than 5 years of age who are stunted from 2012 to 2030
- Child wasting: prevalence of less than 3% by 2030
- Anaemia: 50% reduction in prevalence in women 15–49 years of age from 2012 to 2030
- Breastfeeding: prevalence of exclusive breastfeeding in the first 6 months of at least 70% by 2030
- Child overweight: prevalence of less than 3% by 2030
* The National Nutrition Mission 2022 target for stunting and underweight is for children aged 0–6 years; for consistency and to allow for comparison with the global targets it is estimated here for children younger than 5 years.
† The National Nutrition Mission 2022 target for child anaemia is for children aged 6–59 months; for consistency and to allow for comparison with the global targets it is estimated here for children younger than 5 years.
‡ A relative reduction in the prevalence of stunting is estimated instead of the absolute numbers for consistency with other indicators, because all other targets are based on prevalence.
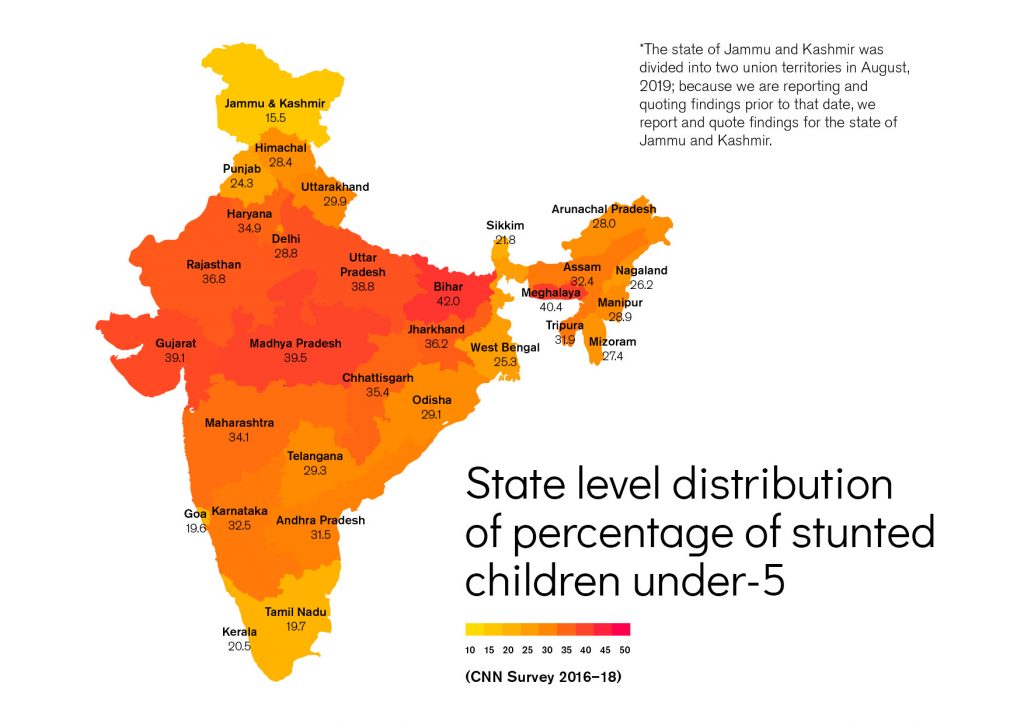
Although the total deaths caused by malnutrition in India declined across all age groups from 36.5% in 1990 to 17.3% in 2017, the accounts of deaths for children under 5 years caused by malnutrition in 2017 were a staggering 68.2%. Of the 1.04 million under 5 deaths in India in 2017, this translates into 706,000 deaths. Child malnutrition persists with more than one in three children under 5 years being either stunted or underweight in India in 2016. The rate of prevalence of stunted children under 5 declined from 48% to 38% between 2006 and 2015, however, in 2016 46.4 million children under 5 were stunted with irreversible consequences for both their physical and cognitive well-being.
The number of wasted children (a measure of acute severe undernutrition with high morbidity and mortality risks) under 5 years old had gone up from 19.8% to 21% between the National Family Health Surveys (NFHS) carried out in India in 2005 (NHFS-3)and 2016 (NHFS-4). The Food and Agriculture Organization of the United Nations (FAO) estimated that in 2018, 25.2 million children under 5 years in India were wasted.
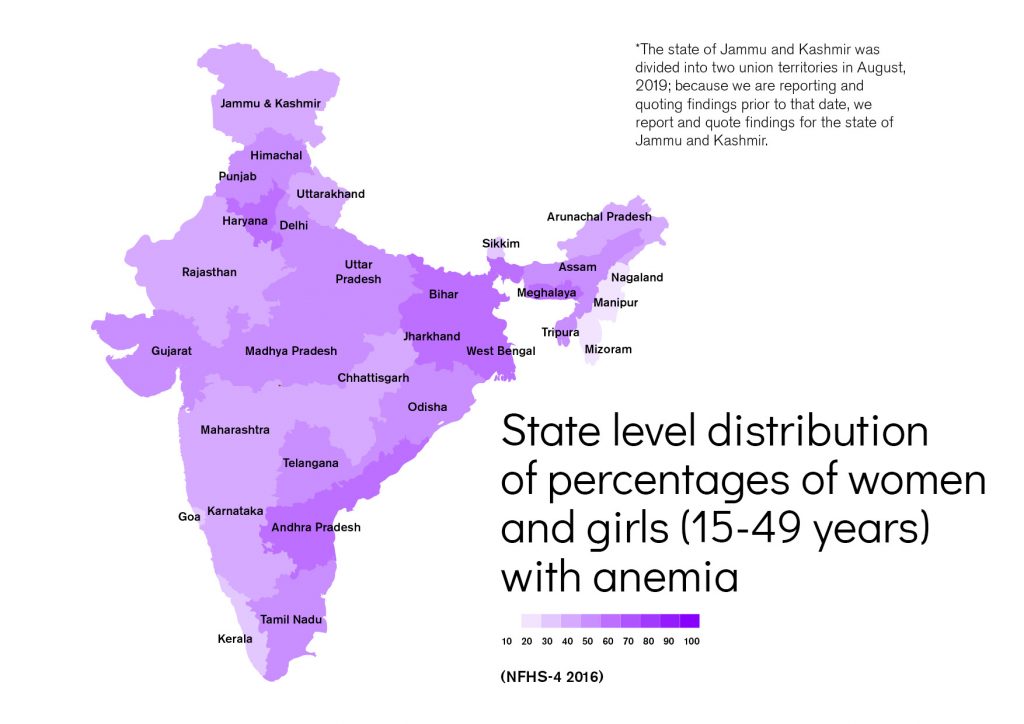
Women and children represent 70% of India’s population. This group is especially prone to suffering from micronutrient deficiencies. Anaemia in India affects 53% of women aged 15-49 years and 22.7% of men. Around 40.5% of children between 6-59 months are anaemic. This makes anaemia a severe public health problem in India among women, adolescent girls and young children. In addition to increased morbidity and negative effects on physical well-being (weakness and/or fatigue), anaemia is associated with delayed mental and psychomotor development and an increased risk of maternal mortality. Poor nutrition, leading to iron deficiency, is the principal underlying factor in more than 60% of all anaemia cases (Kasselbaum, 2016). More than half of all women of reproductive age and children under 5 years in 2017 were anaemic (IIPS, 2017). As shown in Figure 1.1, the estimated 447 million persons with anaemia in India means the country contributes almost one quarter to the global burden, as calculated by the Global Burden of Disease in 2016 (Kasselbaum, 2016).
On the other end of the malnutrition spectrum, the Lancet series on Child and Adolescent Health reports that the prevalence of overweight in children aged 2-4 years was at 11.5% in India in 2017 – an increase of almost 5% since 2010. FAO estimated that 2.4% of children under 5 years old in India were overweight in 2018. Even with the lower estimate, this is particularly concerning as the adverse effects on health and productivity during childhood will persist into adulthood, with a high risk of NCDs such as diabetes and cardio-vascular heart diseases. The projected prevalence of overweight children in India by 2030 is 17.5%. This number is based on trends observed between 1990 and 2017, and is far above the WHO and UNICEF 2030 targets of less than 3% – a target that no state in India is to meet with current annual reduction rates.
For adults, NFHS-4 reports that overweight/obesity affected almost 20.7% women and 18.6% men in 2016, mostly located in urban areas, in wealthier households and among older adults.
Home to almost one-fifth of the world’s population, India has undergone a nutrition transition from an underweight to an overweight population during recent decades (Agrawal, 2002; Dandona, 2017). This has come at significant cost to population health and well-being, and to the already overburdened health systems. In 2016, the five leading causes of disability-adjusted life years (DALYs) in India were ischemic heart disease, chronic obstructive pulmonary disease, diarrheal diseases, lower respiratory infections, and cerebrovascular disease, whilst the top five risk factors for DALYs were child and maternal malnutrition, air pollution, dietary factors, high blood pressure, and high blood glucose (Dandona, 2017).
In India, as globally, NCDs are increasingly prevalent across all socio-economic strata and also contributing more than in the past to premature mortality (Global Burden of Disease study, 2017). As market exposure increases, foods and drinks high in fat, sugar and salt are cheaper and more readily available. The nutrition transition has accompanied a rise in the prevalence of overweight and obesity in India (IIPS, 2017; Luhar, 2017), with an estimated 166 million adults overweight or obese in 2016 (WHO, 2018). They are at risk of diet related NCDs, such as heart disease and diabetes. Furthermore, the dual burdens of undernutrition and overnutrition are becoming more apparent within the same community, household, and among individuals who can be concurrently overweight, stunted and/or micronutrient deficient.
In addition, the prevalence of diabetes is on the rise and is increasingly being diagnosed in children, adolescents and younger adults due to rising levels of obesity, physical inactivity and poor diet.
Given its emergence across socio-economic groups, diabetes is no longer considered to be a disease associated with affluence. In India, it is estimated that 73 million adults are affected by diabetes, the second largest number worldwide (IDF, 2017).
The Government of India has strongly committed to achieving the 2030 Sustainable Development Goals (SDGs). If undernutrition is not effectively reduced, the country will not meet its SDG targets for maternal and child mortality reduction. In addition, if overweight and obesity are not addressed, the burden of NCDs will put a tremendous cost on the development of India and reduce its contribution to global health and economic progress. The current nutrition situation in India justifies its high-level national commitments, with strong policy initiatives based on evidence-informed interventions aimed at combating all forms of malnutrition in the country.
Indian Consumer Behavior
Societal and economic changes are transforming the Indian food landscape, particularly in relation to how companies interact with consumers. Lifestyle changes in India have caused a shift in consumer habits – from the consumption of traditional food to new food habits consisting of increased sugar, fat and salt consumption. A Report of the Working Group on Addressing Consumption of Foods High in Fat, Salt and Sugar (HFSS) and Promotion of Healthy Snacks in Schools of India, constituted by the Indian Ministry of Women and Child Development, highlights that the national sample survey on Nutritional Intake in India 2009-2010 found per capita sugar consumption rose from 22 g/day in 2000 to 55.3 g/day in 2010.
The sample survey found that salt intake ranged between 9 and 12 g/person/day, and total fat consumption increased from 21.2 g/day in 2000 to 54 g/day in 2010. The report also states that India is among the top ten consumers of fast foods in the world. Almost two thirds of the disease burden in India is due to lifestyle diseases with the National Health Policy 2017 recognizing the epidemiology shift of diseases.
Demographically, India has a very young population with 65% under the age of 35, constituting the key drivers of industry growth. With a large young population, an increase in dual income and nuclear families (parents living with their children only) is becoming more prevalent.
Several factors (see above) have been identified which are thought to have led to an increased consumption of products from the fast-growing food and beverage segments in India.
Breakfast Cereals; Savory Snacks; Seasonings, Dressings & Sauces ; Naturally Healthy Beverages; Ready Meals; Confectionery; Organic Food; Dairy Food; Bakery).
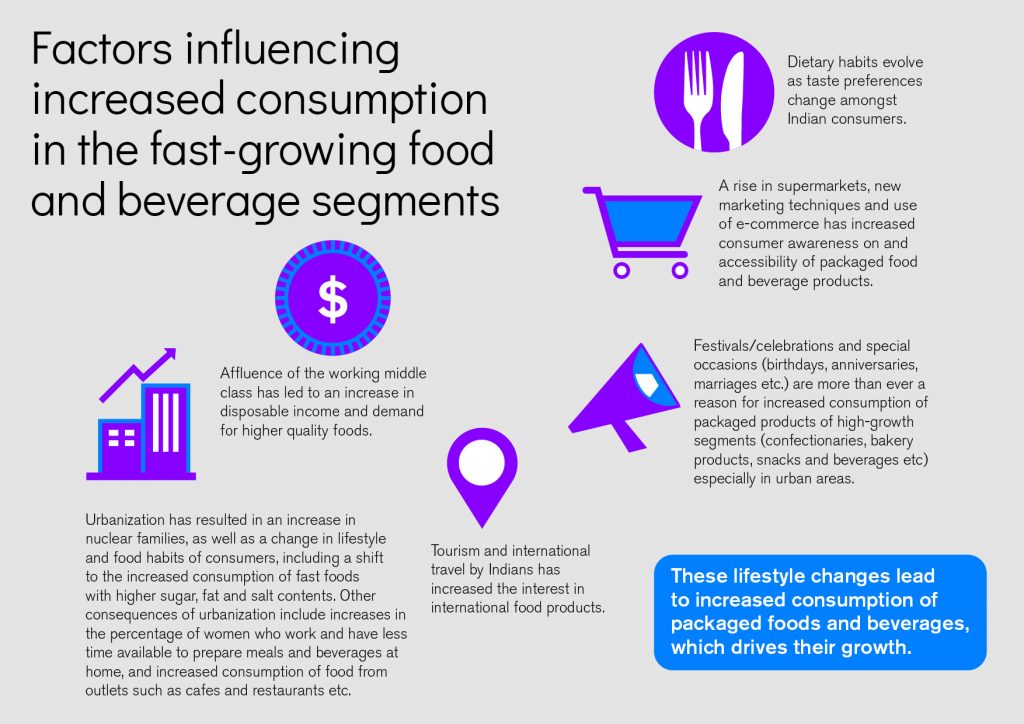
Based on the above factors, combined with India’s strong total consumer base of over 1.25 billion, the opportunity is clear for existing as well as new players in the fast growing food and beverage market to contribute healthier, affordable and tasty products that would improve consumer diets.
The Indian Food and Beverage Industry
India is the seventh fastest growing economy in the world and is becoming one of the leading economic powers. The expected GDP growth rate of India in 2023 is 7.8% and the country is set to be the third largest consumer economy by 2025. With a projected population of 1.3 billion in 2020, the Indian market presents immense potential for further growth and development.
The food and beverage sector is the fifth largest manufacturing sector in India. Between April 2000 and June 2017, the food industry contributed 3.48% to total foreign direct investment equity inflow (USD 7.81 billion) in India. The Indian food market is growing at a rate of 12% annually and is expected to exceed USD 540 billion in 2020.
With significant development in production, processing, distribution and marketing of food and beverages, packaged food is considered a ‘mature market in India’ with a sales retail value of over USD 71 billion in 2018.
The Ministry of Food Processing Industries expects the total value of the food and beverage segment in India to increase to USD 1.142 trillion by 2025. In the India Food Report 2018-2019 by the IMAGES Group, food consumption is estimated to be growing at a compound annual growth rate of 11.6%, with the food retail market rising from USD 403.3 billion in 2016 to USD 552.9 billion in 2017. Food groceries take up more than 90% and the food service market less than 10%, with the latter largely situated in urban areas and the largest cities (the Delhi and Mumbai metropolitan areas account for 20%).
The food processing industry ranks first in the country in terms of the number of operational factories and employment, and operates with a network of over 37,000 processing units spread across the country. Increased production in food segments such as fruits and vegetables but also milk and milk products are benefiting from the growth of the industry.
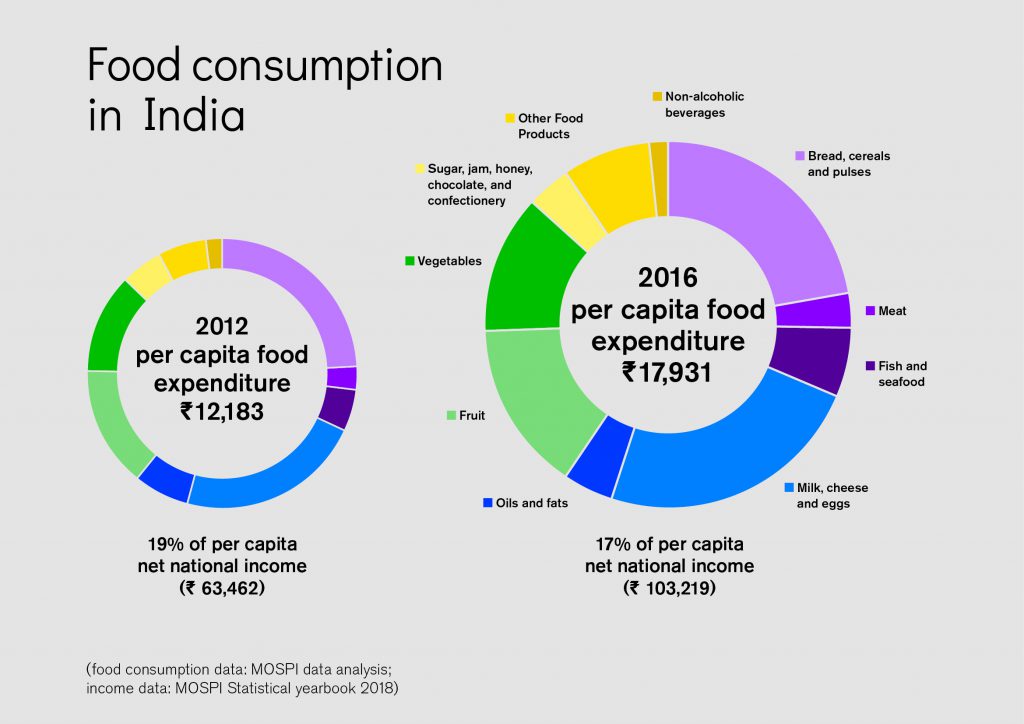
The Per Capita Annual Consumption (PCAC) of various food groups in India has changed substantially in recent times. For example, the PCAC of milk and milk products grew at an annual growth rate of 12% between 2012 and 2016.[iv] Food grocery constitutes a substantial share of Indian consumption, totaling 30% in total in 2016. The distribution of food to consumers involves serving a large fragmented base of kiranashops (small neighborhood retail stores). Around 12-14 million of these unorganized retail stores are spread over 5,000 towns and 600,000 villages across India. But modern grocery retailers appear to be slowly gaining share from traditional retailers.
Different initiatives have been undertaken to support the agri-food sector in India. Also, the rise of regional brands has contributed to industry growth in several states linked to distinct culinary taste preferences. Initiatives such as Make in India, Startup India, Digital India, Ease of Doing Business and reforms on foreign direct investments have contributed to increasing investor confidence in India. In 2017, the Government of India launched a Scheme for Agro-Marine Processing and Development of Agro-Processing Clusters (SAMPADA) with the aim of modernizing infrastructure – from the farm to retail outlets – towards more efficient supply chain management.
Food Regulations
In 1993, the Government of India took important steps to address malnutrition by introducing the National Nutrition Policy. In 2006, the Food Safety and Standards Act transformed the way of thinking about food safety in India. The Act lays down evidence-based standards that consolidate various acts and legislations into one reference point. In 2016, eight Standard Review Groups were set up to ensure standards are up-to date with national and international demands. In 2017, the National Health Policy aimed to inform, clarify, strengthen and prioritize the role of the Government in creating health systems. Another crucial step towards better nutrition in India was the launch of the 2018 National Nutrition Mission/ POSHAN Abhiyaan, which outlines clear targets towards reducing malnutrition and is supported by substantial budgets and campaigns like ‘Eat Right India’. Bollywood actor, Rajkummar Rao, became the spokesperson of the Eat Right India movement with the tagline Aaj se thoda kam (from today, slightly less) to urge people to reduce their salt, sugar and fat intake.
The Food Safety and Standards Authority of India (FSSAI) sets guidelines and standards and works with many stakeholders active in the food system. With recent revisions to the Food Safety and Standards (Packaging and Labeling) Regulation, 2011, a new regulation proposes that packaged food companies declare nutritional information, including the levels of saturated fat, trans-fat, added sugar and sodium per serving, on the front-of-pack labeling. Several food companies have pledged to voluntary commit to reducing salt and sugar in their products by 2020.
FSSAI also introduced food safety display boards in restaurants and food retail stores to educate consumers, and formulated guidelines for high fat, salt and sugar foods. Further actions by the Authority to reduce malnutrition include dietary diversification, engagement with the private sector in food fortification, nutritious food campaigns, and emphasizing social determinants of nutrition.
In the last 3 years, FSSAI strengthened the regulatory environment and encouraged and supported improved compliance with these regulations. For example, in December 2017, FSSAI established a self-regulation platform, the Responsible Food Companies Score (ReFoc Score), for food companies, retailers stocking packaged food and fast-food restaurant chains.
Initiatives such as the Vision of India’s 2022 National Nutrition Strategy – Kuposhan mukt bharat (free from malnutrition, across the life cycle), the Integrated Child Development Scheme, Maternity Benefit Programme (Pradhan Mantri Matru Vandana Yojana (PMMVY since 2016), Mid-Day Meal Scheme (since 1984), and POSHAN Abhiyaan (since 2018), are aimed at reducing child and maternal malnutrition. Some IT solutions, such as the Indian Food Laboratory Network, the Safe and Nutritious Food Initiative (SNF), and the Food Smart Consumer Portal are meant to develop social and behavioral changes amongst the Indian population.