The Global Context
The state of overweight and obesity in the world
Overweight and obesity are the most widespread forms of malnutrition globally: these conditions, defined by a body mass index (BMI) equal to or greater than 25 and 30, respectively, are associated with a greater number of deaths worldwide than undernutrition. In every region of the world, apart from sub-Saharan Africa and Asia, there are more people living with obesity than those who are underweight.
The number of people who suffer from overweight and obesity has nearly tripled since 1975 and keeps rising, In 2016, 13.1 percent of the global adult population was overweight or obese, an increase from 11.8 percent in 2012. Once thought to be a high-income country issue, today overweight and obesity affect most countries in the world, with over 70 percent of adults living with obesity found in low- or middle-income countries.
Child obesity is witnessing similar upward trends. In 2019, 5.6 percent of the world population under the age of 5 was overweight or obese, a slight increase since 2012. This trend represents a challenge for Global Nutrition Target 4, which aims to put an end to the rise of overweight children by 2025. Only four years away from this target date, the world is not on track to deliver on it.
According to estimates by the Potsdam Institute for Climate Impact Research, by 2050, 45 percent of the world population will be overweight or obese. Several reasons can account for the dramatic increase in the prevalence of obesity. Increasingly sedentary lifestyles have been accompanied by a greater availability of calorie-rich foods without increased access to healthier food options: food supply chains have been geared to supply quantity calories rather than nutrients. As a result of rising consumption of energy-dense, nutrient-poor diets, overweight and obesity today are also associated with poorer micronutrient status. This calls for actions that target overweight and obesity not as stand-alone issues, but as the result of systemic failures in the global provisioning of healthy diets.
The nutrition transition
Originally theorized by American academic Barry Popkin in the 1990s, the nutrition transition indicates changes of dietary patterns – determined by economic developments and food processing techniques – from ‘collecting food’ to ‘famine’, ‘receding famine’, ‘degenerative diseases’ and finally to ‘behavioral changes’, the last pattern being defined by the desire to improve health.
Plenty of evidence today supports the concept of a nutrition transition towards global diets with high intakes of increasingly available and affordable nutrient-poor, calorie-rich foods (i.e. the ‘degenerative diseases’ phase). This transition, the result of income growth, demographic changes, urbanization and new patterns of food distribution, is associated with rising proportions of the global population suffering from overweight, obesity, and diet-related non-communicable diseases.
There is initial evidence suggesting that diets rich in ultra-processed foods (UPFs) – which are rapidly rising in low- and middle-income countries and are already a significant proportion of the diets in some high-income markets such as the US, Canada and the UK – are associated with higher risk of obesity, diabetes and other diet-related diseases. The rising consumption of these highly palatable and cheaply available foods denotes the current stage of the nutrition transition. A better understanding of the relationship between the level of food processing and product healthiness, as determined by a robust Nutrient Profiling Model (NPM), is needed to establish which characteristics of UPFs of low underlying nutritional value can represent a risk to public health.
There is yet no evidence, however, to support the theory of a widespread, global transition to dietary patterns aimed at improving health outcomes. To ensure that the last stage of the transition does occur, there is a need to ensure that nutrient-rich foods are not only available, but also affordable, appealing, and aspirational.
The impact of COVID-19 on overweight and obesity
The relationship between COVID-19 and obesity has been extensively researched since an association between obesity and worse health outcomes of the novel coronavirus was first detected in early 2020. A March 2021 study by the World Obesity Federation provides a detailed account of how overweight and obesity have been significant factors in determining risks of hospitalization, intensive care, and death from COVID-19 globally. In countries where less than half of the national population is overweight, the likelihood of dying from COVID-19 has been about a tenth of that seen in countries where the majority of the population is overweight.
The COVID-19 and overweight/obesity relationship, however, is not unilateral. As a result of lockdown restrictions worldwide, new trends such as increased snacking, stress eating and reduced exercise have triggered experts’ warnings about potential increases in adult obesity.
Similarly, all forms of child malnutrition, including obesity, are expected to worsen as a result of the pandemic: lockdown eating and school closures have significantly deprived children of healthy eating and exercising routines. A closer monitoring of obesity trends post-pandemic will be needed to fully understand the magnitude of this impact.
The state of undernutrition in the world
In 2019, 690 million people, or 8.9 percent of the global population, were undernourished, and 2 billion people were food insecure – these numbers have been rising since 2014 and will continue to rise, partly as a result of the COVID-19 pandemic.
Amongst the categories of people most vulnerable to undernutrition are children: in 2019, 21.3 percent of children under 5 years of age were stunted, or too short for their age, and 6.9 percent were wasted, or too thin for their height. Stunting and wasting are two different manifestations of undernutrition and can, respectively, lead to impaired physical and mental development and heightened risk of death.
The growth in global prevalence of undernourishment, as well as in food insecurity witnessed in recent years, marks the continuation of the trend of rising hunger which started in 2014, when decades-long progress towards achieving SDG2 Zero Hunger started being reversed. As a result of conflict, poverty, and climate change, the world was not on track to achieve SDG2 by 2030 before Covid-19. Compounded by the economic fallout of the pandemic, conflict and climate extremes are exacerbating the already dire state of undernutrition globally. In March 2021, a joint statement by the United Nations Food and Agriculture Organization (FAO) and the World Food Programme (WFP) warned that 34 million people are in the emergency phase of food insecurity, or ‘one step away from starvation’.
To fulfil the global sustainable development agenda and meet the Global Nutrition Targets, efforts to combat undernutrition must increase significantly.
The cost of a healthy diet
Several metrics exist that assess hunger worldwide: The Prevalence of Undernourishment, the Food Insecurity Experience Scale, the Integrated Food Security Phase Classification and many more. Whilst measures of hunger are necessary to understand the scope of undernutrition, in recent years new metrics have been used to assess the scope of malnutrition as a whole. Among these is the cost of a healthy diet.
A healthy diet is not only one that provides sufficient energy, but also one that balances energy intake with energy expenditure through an active lifestyle, one that provides all nutrients and micronutrients needed to nourish the human body and one that has a certain degree of dietary diversity.
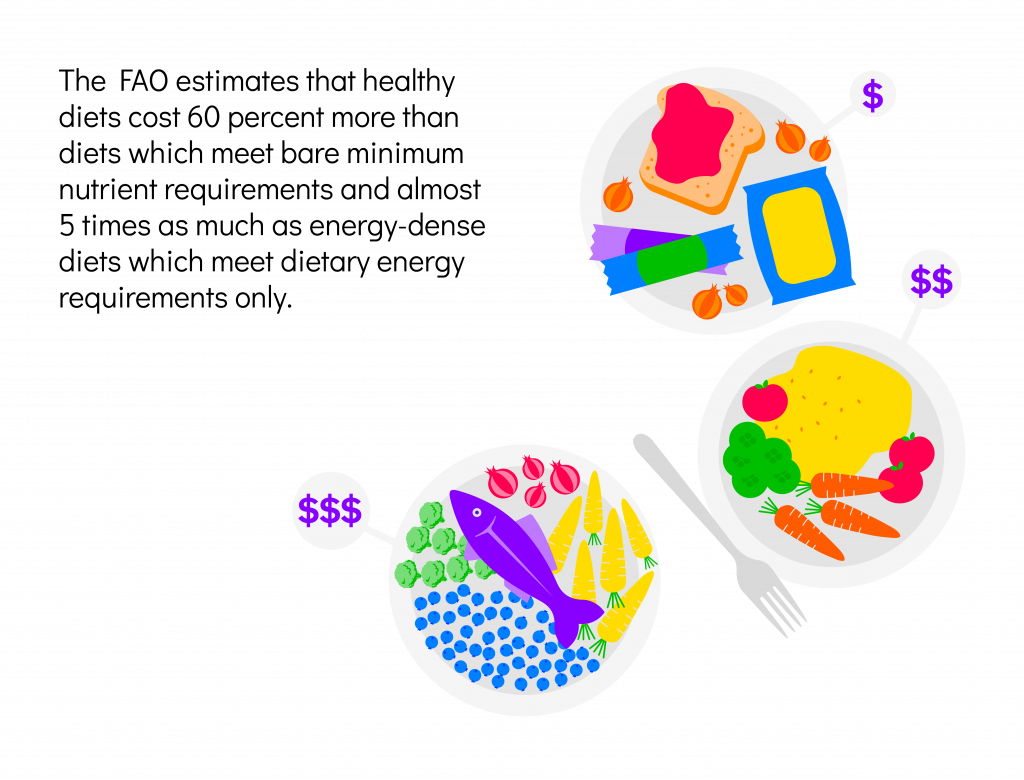
The FAO estimates that healthy diets cost 60 percent more than diets which meet bare minimum nutrient requirements and almost 5 times as much as energy-dense diets which meet dietary energy requirements only – this trend is witnessed in all regions of the world, although it affects a greater percentage of the population in low- and middle-income countries where people spend a greater proportion of their income on food. At the global level, this has resulted in 3 billion people not being able to afford a healthy diet and 1.5 million people not being able to afford a merely nutrient-adequate diet.
The impact of COVID-19 on undernutrition
The dramatic effects of the COVID-19 pandemic on food and nutrition security are, by now, well documented.
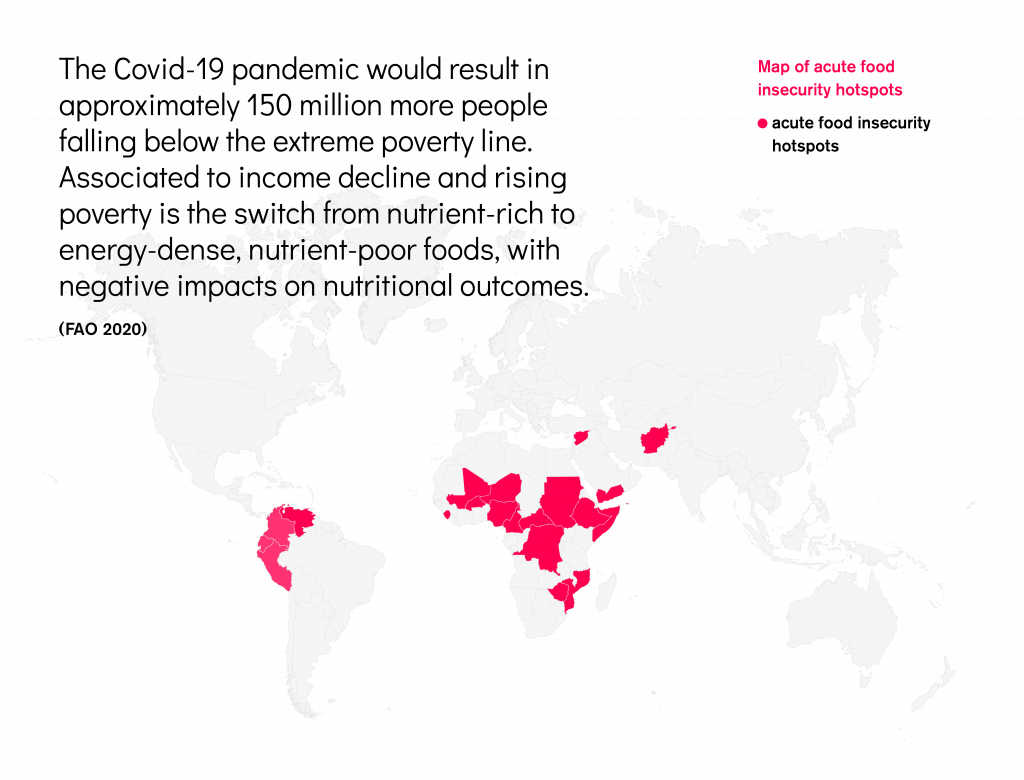
In July 2020, the FAO estimated that COVID-19 might increase the number of undernourished people in the world by anything between 83 and 132 million, depending on prospects for global economic recovery. Estimates made at the early stages of the pandemic, however, may no longer be accurate, as new evidence shows that pandemic effects might reach further than expected. A December 2020 study by the International Food Policy Research Institute (IFPRI), for instance, estimated that the COVID-19 pandemic would result in approximately 150 million more people falling below the extreme poverty line. The switch from nutrient-rich to energy-dense, nutrient-poor foods is associated with income decline and rising poverty with negative impacts on nutritional outcomes.
As the economic and health consequences of the pandemic continue to unfold, it becomes clearer that women and children are especially vulnerable and increasingly likely to be affected by a deteriorating nutritional status. It is estimated that, by 2022, the pandemic might lead to a 9.3 million and a 2.6 million increase in wasted and stunted children, respectively, as well as 168,000 additional child-deaths and 2.1 million maternal anemia cases. Significant investments will be needed to minimize the effects of the pandemic.
The state of micronutrient deficiences in the world
Micronutrients such as iron, vitamin a, vitamin d, iodine, folate and zinc are fundamental to full physical and mental development, yet they are missing from the diets of many in the world: over 2 billion people globally suffer from micronutrient deficiencies. Micronutrient deficiency, also known as hidden hunger, is especially common amongst low-income populations and more prevalent in regions and countries with low dietary diversity. Hidden hunger affects people who suffer from overweight or obesity and people who are undernourished.
Amongst the populations most vulnerable to hidden hunger are women and children. At least 1 in 2 children globally lacks essential micronutrients in their diets, and as many as 528 million women, including both pregnant and non-pregnant women, suffer from iron deficiency alone.
Large-scale food fortification (LSFF), either through bio-fortification of crops or through the fortification of food products ready for human consumption, has proved to be a cost-effective tool to tackle micronutrient deficiencies. It is estimated that for every dollar spent on fortification there is a US$27 return from outcomes of improved nutrition.
Salt iodization: the public health success of public-private partnerships
Iodine is a diet-derived mineral that contributes to the well-functioning of the body by creating thyroid hormones which are necessary throughout life and especially during pregnancy and infancy for full brain development. Preventable mental impairment, such as loss of learning ability and cretinism, as well as disorders such as stillbirth and miscarriages, can result from even low levels of iodine deficiency.
Salt iodization is a form of large-scale food fortification, whereby food-grade salt for human consumption is fortified with iodine. Thanks to public-private partnerships aimed at universal salt iodization, iodine deficiency has been greatly reduced: 86% of the world’s households now have access to iodized salt, 129 countries worldwide have adopted mandatory salt iodization programs, and only 20 countries globally have insufficient iodine status, compared to 113 in the 1990s.
The successes of universal salt iodization programs has been one of the first signs indicating that food fortification can be an efficient and cost-effective tool to tackling malnutrition globally, and it would not have been possible without public-private partnerships involving the food industry: ‘Universal salt iodization has been one of the great public health success stories of the last 25 years’ – Werner Schultink, Executive Director, Iodine Global Network.
The impact of COVID-19 on micronutrient deficiencies
The impact of COVID-19 on access to micronutrients is at least threefold.
Firstly, as a result of the economic fallout caused by the pandemic, people worldwide have switched from nutrient-rich to energy-dense, nutrient-poor foods, thus reducing their dietary diversity and access to foods rich in micronutrients.
Secondly, by negatively affecting global food supply chains and international trade, which food fortification programs inevitably rely on, through export restrictions and rising costs of freight, COVID-19 has reduced the reach and scope of food fortification programs in low- and middle-income countries, as reported by the Global Alliance for Improved Nutrition (GAIN).
At the same time, lockdown restrictions have hindered nutrition services, including services providing micronutrient supplementation: as many as 100 million children have missed a dose of vitamin A supplementation in 2020 as a result of pandemic management measures.
The importance of a healthy start in the first 1,000 days
Optimal nutrition during the time between conception and the second birthday of a baby – the first 1,000 days – are fundamental to children’s development, in terms of their health, and physical and cognitive abilities. With breastmilk being a free, safe source of all necessary nutrients and antibodies, breastfeeding has long been understood to be the best and most effective way to nourish infants while also reducing their susceptibility to overweight and obesity.
The World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommend that infants be exclusively breastfed for the first six months of their lives, when appropriate complementary foods can be introduced, while breastfeeding continues for two years or beyond. However, the world is currently not on track to meet Global Nutrition Target 5 which is to increase the global rate of exclusive breastfeeding in the first six months to 50% by 2025. In 2019, only two in five children globally were exclusively breastfed at this crucial phase of their lives. The 2019 Cost of Not Breastfeeding tool shows as many as 593,379 childhood deaths (0 to 23 months) from diarrhea and pneumonia are attributable to not breastfeeding according to the global WHO and UNICEF recommendations, and that optimal breastfeeding has the potential to prevent an additional 98,243 deaths of mothers annually from cancer and type II diabetes.
The WHO identifies inappropriate marketing of breast-milk substitutes (BMS) as one of many factors that negatively impacts breastfeeding rates worldwide. To limit the impact of BMS marketing, in 1981, the World Health Assembly (WHA) adopted the International Code of Breast-milk Substitutes (known as The Code), that makes a series of recommendations to member states and BMS manufacturers and distributors. Since that date, 18 further WHA resolutions have been passed that reinforce, revise or extend the provisions of the 1981 Code (collectively referred to as The Code). However, as of 2020, 30% of countries still have none of its provisions in their law and only 31 countries have legal measures that implement the full breadth of The Code’s recommendations.
ATNI’s research on the extent to which major manufacturers of BMS and complementary foods comply with The Code can be found here.
The BMS/CF Marketing Index 2021
The BMS/CF Marketing Index, published in June 2021, assessed the marketing practices of the world’s nine largest BMS and CF manufacturers, six of which are also part of the Global Index 2021 (Danone, FrieslandCampina, KraftHeinz, Mengniu, Nestlé, and Yili).
The assessment examines the extent to which these companies market their BMS and CF products in line with The Code. The research entails two components: i) BMS/CF 1: an analysis of companies’ BMS/CF marketing policies, management systems and disclosure and ii) BMS/CF 2: two in-country assessments of companies’ marketing practices on the ground (the Philippines and Mexico in 2020). The total possible overall BMS/CF Marketing Index score is 100%. The higher the score, the closer the company has come to achieving full compliance with The Code. An adjustment proportionate to this score is then calculated to be applied to each of the six companies’ Global Index score, reflecting the importance of corporate focus on infant and young child nutrition. The adjustment depends on which elements each company has been scored on. For Danone, FrieslandCampina, KraftHeinz, and Nestlé the maximum adjustment that can be made is -1.5, as in the 2018 Global Index. The maximum adjustment to the Global Index 2021 score for Mengniu and Yili is -0.75 as it was only possible to assess these two companies on BMS/CF 1.
Overall, the findings reveal that 40 years after the adoption of The Code, the world’s largest baby food manufacturers continue to fall short of meeting its recommendations.
Impact of COVID-19 on breastfeeding
Initial uncertainty about the safety of breastfeeding during the COVID-19 pandemic led to concerns about whether mothers could transmit the virus to their infant through breastfeeding. In June 2020, however, the WHO issued a statement encouraging mothers to continue breastfeeding, even when suspected or confirmed with COVID-19 infection.
With experts warning about the consequences of the spread of misinformation, initial concerns and uncertainty are likely to have had a negative impact on breastfeeding rates. A study of 33 national guidelines for infant care by Alive & Thrive (A&T) found that none of the documents analyzed fully aligned with the WHO breastfeeding and COVID-19 guidelines. Similarly, a January 2021 study by (A&T) and FHI 360 of nine companies in 14 countries found instances of violations of The Code in the wake of the pandemic.
The long-term impacts of less breastfeeding during this time could be significant: estimates indicate that a mere five percent reduction in breastfeeding could lead to an additional 16,469 child deaths in low- and middle-income countries. It is therefore of the utmost importance to support breastfeeding and monitor compliance with The Code throughout the COVID-19 pandemic, and beyond.
A compelling case for the food and beverage industry
Malnutrition in all its forms is a leading cause of death worldwide: in 2017, 11 million deaths and 255 million disability-adjusted life years were attributable to dietary risk factors. Globally, 45 percent of deaths among children under the age of 5 are linked to undernutrition. Tackling malnutrition is thus a moral imperative, which is necessary to reduce diet-related illnesses and deaths.
Tackling malnutrition is also an economic imperative. Overweight and obesity, undernutrition and micronutrient deficiencies, indeed, represent a heavy burden to economic development globally: their material cost is estimated at 5% of global income or US$3.5 trillion per year. The economic cost of malnutrition differs widely by country and by region. Whilst undernutrition is significant in world regions such as Africa and Asia, where it accounts for an 11% loss of GDP each year, overweight will lead to an annual 3.3% reduction in GDP in Organisation for Economic Co-operation and Development (OECD) countries and will constitute as much as 8% of national health expenditure.
The COVID-19 pandemic has exacerbated the cost of malnutrition, with estimates indicating that, by 2022, COVID-19 will have resulted in US$29.7 billion worth of productivity losses derived from increased rates of childhood stunting, wasting and mortality.
What cannot be determined with exact precision, however, is the social cost of malnutrition. Poor diets negatively impact neurodevelopment, with dramatic consequences on children’s academic performance, careers and earning prospects. General well-being, including mental health, is also hindered by malnutrition. Children who are overweight, for instance, are more likely to be bullied, which can result in adverse mental health outcomes.
The largest global food and beverage manufacturers were facing a number of challenges even before the COVID-19 pandemic with mounting evidence of consumer demand increasingly shifting towards smaller challenger brands with a purpose-driven outlook, as well as towards cheaper private label brands – trends which are predicted to continue after the pandemic. Anticipating changes emerging from both consumer pressure and regulatory measures, CEOs of food and beverage companies worldwide had acknowledged the need for their industry to play a role in promoting healthier lifestyles even prior to the COVID-19 pandemic.
In the rapidly-evolving context of the pandemic, food and beverage manufacturers have been faced with new challenges, including the responsibility of feeding the world at a time of crisis. As an essential industry, the packaged food industry has benefitted from the pandemic, registering a year-on-year retail value growth of over 5% between 2019 and 2020. On the one hand, indeed, food companies – from small to large, from local to transnational – have been struggling with disruptions in distribution channels, transport restrictions and changing consumer demand.
On the other hand, in many instances, they have been able to adapt to this challenging environment and to innovate rapidly. As highlighted in recent IFPRI research, the pandemic has outlined both fragility and resilience in food supply chains. The ability of the food and beverage sector to innovate has resulted in significant changes in food environments. E-commerce in food retail, for instance, has witnessed a nearly 50% growth worldwide and has increased by over 100% in several middle-income countries.
The reach and market penetration of the packaged foods industry – with a retail value of nearly US$2.5 trillion in 2020 – speaks for the magnitude of the impact the industry could have on nutrition globally: food and beverage manufacturers reach virtually every individual on the planet. Further, the rapid expansion of the industry in emerging markets in the Asia-Pacific, Latin America, and Middle East and Africa regions – which represent the main drivers of growth for the industry – presents the opportunity to reach populations who are vulnerable to malnutrition.
There are several business risks linked to the production of products that contribute to poor diets: reputational risks, litigation risks, risks of losing out on emerging markets for healthier products, and regulatory risks. The latter have been increasingly brought under the spotlight by nutrition stakeholders in the past years. As the evidence about the drag of poor diets on national health spending increases, governments continue to regulate food environments. To date, for instance, 44 sugar taxes exist globally. In addition, several governments worldwide have implemented, or are considering implementing more stringent regulations with regards to matters such as front-of-pack food labelling and advertising of unhealthy food products. This represents a strong material risk for investors with holdings in global food and beverage manufacturers, insofar as companies with a product portfolio rich in foods that are high in fat, salt and sugar (also known as HFSS foods) could see decreasing sales and revenues.
The cost of malnutrition represents a burden not only for national governments worldwide, but also for the private sector more directly. A July 2020 report by Chatham House shows that multinational corporations, across different sectors, lose, annually, an estimated US$8–38 billion from reduced worker productivity due undernutrition, an estimated US$4–27 billion due to overweight and obesity and an additional 0.8 percent of GDP due to anemia (in the countries where the condition was studied). Thus, tackling malnutrition in all its forms can be viewed as a tool to achieve business growth.
However, food and beverage manufacturers are becoming more engaged with the topic of nutrition as the number of private sector accountability mechanisms increases, as business risks linked to malnutrition become more evident, and as opportunities arising from promoting healthier diets become more visible.
COVID-19 enhances the business case for nutrition
The COVID-19 pandemic has brought the role of the food industry in tackling obesity and other diet-related diseases, which are risk factors for COVID-19 infection and mortality, under the spotlight and has highlighted the relevance of healthy diets for public health.
On the one hand, the pandemic has resulted in a greater level of awareness of nutrition, amongst both governmental bodies and consumers. Governments around the world are rolling out stricter regulations for less healthy foods as a preventive healthcare policy, particularly aimed at tackling obesity. At the same time, sales data shows that COVID-19 has accelerated rising demand for healthy food products by relatively affluent consumers. As highlighted in ATNI’s second COVID-19 report, the COVID-19 pandemic is accelerating the increase in the demand of healthier products: affluent consumers are becoming increasingly engaged with the topic of nutrition and wellbeing. Analysis from Euromonitor International shows that ethical concerns are becoming increasingly important to consumers, who expect businesses to perform well both on environmental and social issues such as health.
As a result of COVID-19, the health and wellness packaged food category witnessed an almost unprecedented single-digit value growth at the global level, which is forecast to last beyond the pandemic.
On the other hand, as outlined throughout this chapter, the COVID-19 pandemic is resulting in reduced access to healthy and nutritious foods for poorer populations and, in some cases, to increased demand for less healthy food products such as snacks and comfort foods.
At the intersection of the trend outlined above lies a unique opportunity, and responsibility, for food and beverage manufacturers to grow and innovate by putting the well-being of their consumers first – a process which the Global Access to Nutrition Index aims to facilitate.